
Plantar Fasciitis—Asheville, NC
Walk & Run with Ease Again
Mornings are tough for many people, but that’s especially true for those suffering from plantar fasciitis. If you regularly experience stabbing pain on the bottom of your foot near your heel, then it’s time to visit Asheville Non-Surgical Orthopedics. Dr. James Pinkston has diagnosed and successfully treated many patients with this condition, helping them recover the daily comfort and function they deserve. If you’re ready to make your foot pain go and stay away, click here to schedule a consultation.
What is Plantar Fasciitis?
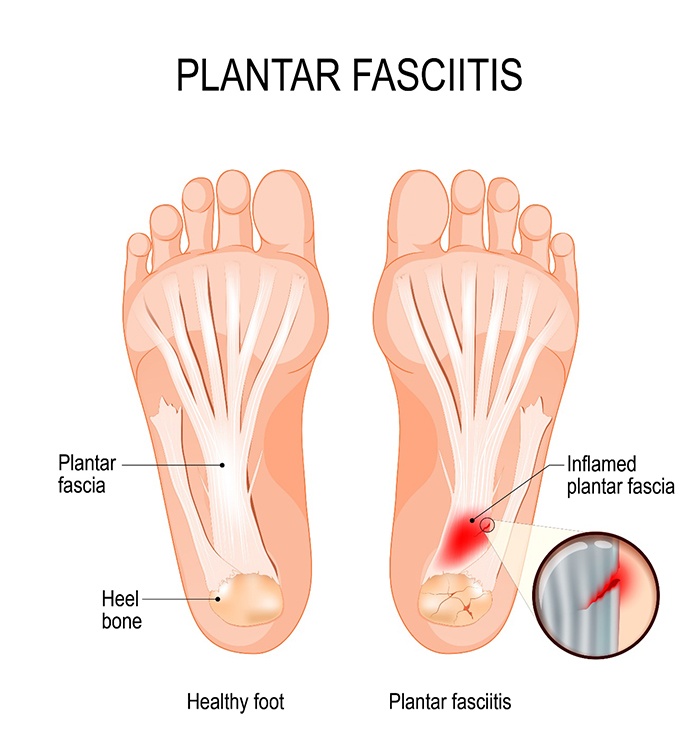
Running from your heel to your toes along the bottom of your foot is a thick band of tissue called the plantar fascia. Essentially, it serves as a shock absorber as you walk or run, supporting the arch of your foot. If it is exposed to excessive pressure or is overstretched, it can develop small tears that can become irritated and inflamed. This is the root source of the pain associated with the condition.
What Are the Symptoms of Plantar Fasciitis?

The primary symptom of plantar fasciitis is extreme pain felt on the bottom of the foot when walking or running. Typically, it is worst after an extended period of rest, which is why most patients tend to have the most severe pain after getting up in the morning. As the day goes on, this pain will usually dissipate, but it can return after standing for many hours or sitting for a while and then standing.
What Causes Plantar Fasciitis?

A multitude of factors can increase the risk of someone developing this condition, including:
- Age: People between the ages of 40-60 have a higher chance of experiencing plantar fasciitis.
- Certain Physical Activities: Running (particularly over long distances) and strenuous dancing are commonly associated with plantar fasciitis.
- Shape of the Foot: Having flat feet, high arches, or even an atypical pattern of walking can place undue stress on the foot that leads to injury.
- Obesity: Simply put, extra pounds put more stress on the feet and make it easier for the plantar fascia to become injured.
- Jobs That Involve Standing: Construction workers, those in manufacturing, teachers, service staff, and others who spend most of the day on their feet can easily develop plantar fasciitis.
How is Plantar Fasciitis Diagnosed?

The symptoms of plantar fasciitis are very distinct, but in order to make sure it’s the cause of a patient’s problems, Dr. Pinkston will perform a physical exam and may take X-rays and use diagnostic ultrasound to rule out any other issue that could create pain in the foot (like a small fracture or bone spur).
How is Plantar Fasciitis Treated?

There is a wide array of treatments that have been shown to successfully eliminate plantar fasciitis. In addition to prescribing pain medication to offer immediate relief, Dr. Pinkston may recommend that a patient wear a certain type of shoe or use orthotics to help their feet get the support they need.
For more advanced cases, corticosteroid injections can quickly alleviate pain, and then PRP therapy, prolotherapy/Prolozone, or biologic cell therapy can help accelerate healing. Surgery is not necessary most of the time, but it may be recommended if a patient doesn’t respond to other treatments.
Plantar Fasciitis FAQs

While there is a lot of useful information on this page, you may still have questions about plantar fasciitis, and you deserve to have as much information as possible before deciding on your care. That’s why our team has answered a few more popular questions on this topic below. To get in touch to ask anything we haven’t already covered, be sure to give us a call.
How can I tell if I have plantar fasciitis?
The most definitive sign is that you will experience pain and stiffness in the heel. It can be just a dull ache or even a sharp or burning sensation. You may notice these symptoms after a certain activity, in the morning, or after standing or sitting for a long time. And, they will tend to get worse over time without treatment.
Can plantar fasciitis heal on its own?
With adequate rest, yes, plantar fasciitis can fully heal. However, taking the time required is often not feasible for most people, as the problem stems from their job or sports. This is why non-surgical orthopedics is so helpful—they enable a patient to get the treatment they need while keeping any downtime to a minimum.
How long does plantar fasciitis treatment take?
It entirely depends on the extent of the condition. If a patient comes to see us right after their plantar fasciitis develops, then they may experience an abatement of symptoms in a matter of weeks. But, for those who have dealt with the condition for a long time, the tissue is quite damaged, so treatment may take several months or need to be ongoing.
What is the quickest way to stop plantar fasciitis pain?
Icing is typically the fastest way to relieve plantar fasciitis pain, as it can help reduce the inflammation. Many people fill up a water bottle and allow it to freeze overnight, as this can fit easily into the arch of the foot. While icing has its place, it’s important to remember that it reduces the pain but does not help with the source of the problem…that’s where treatments like PRP and biologic cell injections can help by stimulating accelerated healing.
Can stretching help with plantar fasciitis?
Yes, but it needs to be done correctly in order to avoid causing additional pain or damage. One stretch that is often recommended involves propping the toes against a wall while keeping your arch and heel flat. This position can be held for 10 seconds and repeated about three to four times a day. Stretching can help make the fascia more flexible and also strengthen the foot muscles, so it is often an essential part of ongoing treatment.